Project Description
KRM’s present day Chief Operating Officer, Jack Shaffer, served as the CIO of The Community Health Network of West Virginia (CHNWV) when it began its implementation of the Indian Health Services Resource Patient and Management System (RPMS) EHR – a derivative of the Veterans Administration’s VistA EHR – to its member rural health clinics in 2006. Shaffer led the deployment of the centrally hosted RPMS-EHR system to nearly 50 clinical locations throughout the state of West Virginia. In four years, the system grew to contain more than 190,000 unique patients, (over 10% of West Virginia’s total population) making it one of the largest EHR’s deployed in the state at that time.
One of the major goals regarding the implementation of the RPMS-EHR system was health improvement. It is important to recognize that an EHR is simply a tool that, if used properly, can enable health care providers to deliver higher quality healthcare. To realize the full potential of a comprehensive EHR, its adoption must be part of a strategic plan to promote an integrated, patient-centered continuum of care. An EHR is an effective tool for improving coordination of care through faster and more accurate communication across care settings and between clinicians and patients. However, the EHR does not change practice by itself, and workflows must be designed to support the use of valuable information contained in the EHR.
As part of CHNWV’s focus on using the RPMS-EHR as a health improvement tool, the creation of a robust data warehouse / business intelligence platform was commissioned and spearheaded by Shaffer. This required the creation and use of advanced data extraction and transformation tools to obtain the clinical data necessary from the RPMS-EHR system as this functionality did not exist within the application itself.
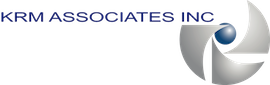
The effort was done in cooperation with a clinical committee comprised of medical practitioners from the various clinics in order to allow member health centers to easily report on standardized clinical quality outcomes and measures. One such measure involved diabetic patients whose HgBA1c lab results were “under control”. (See Figure 1) These clinical dashboards allowed providers to analyze patient data as a population as well as benchmark those measures over a period of time to analyze changes in clinical outcomes. The dashboards also allowed providers to quickly identify specific patients out of compliance or requiring additional levels of care.
The data warehouse created had the capability to perform longitudinal analysis of the clinical measures over varying timescales, which allowed for the observation of trends across the data. (See Figure 2)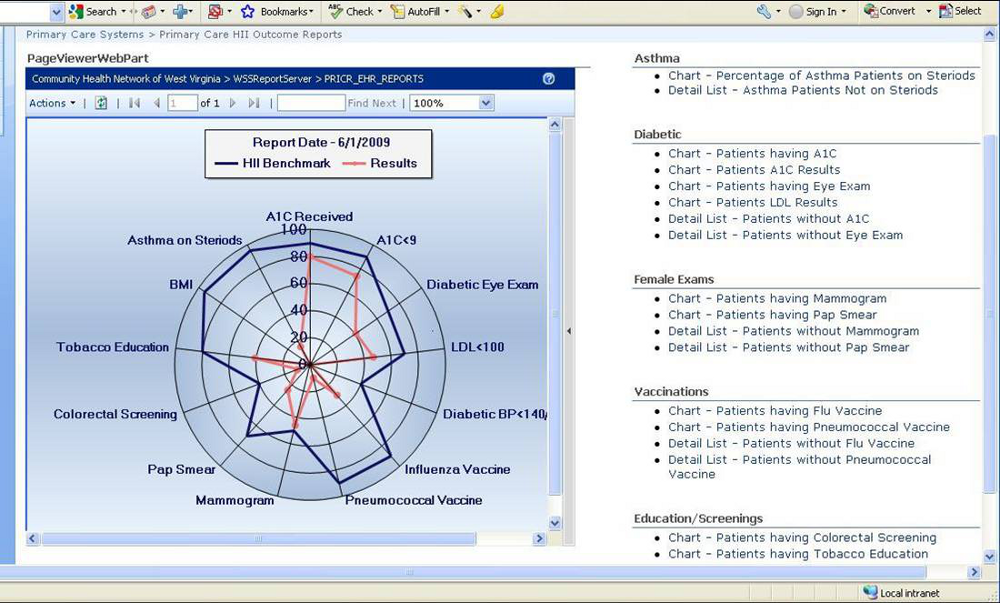
The clinical data warehouse was enhanced further to allow member health centers to report on 24 clinical outcome measures in conjunction with a patient centered medical home initiative being led by the West Virginia Health Improvement Institute (WVHII). These clinical measures were required to be reported to the WVHII electronically. Out of 20 organizations, only 3 were able to report all 24 measures electronically – with CHNWV being one.
CHNWV also compared these actual WVHII clinical outcome measure results to National Committee for Quality Assurance (NCQA) standard benchmarks in an effort to continue to improve clinical outcomes for the patients of member health centers. Many of these same outcome measures became part of the Clinical Quality Measures (CQM) required by eligible providers (EPs) to report in conjunction with meeting Meaningful Use.
While Meaningful Use is a fairly new requirement, the past use of an EHR for quality improvement as well as the work surrounding the reporting of clinical quality measures demonstrates that KRM Associates has the personnel necessary to extract, transform and synthesize clinical data from electronic medical record systems for use in the health improvement process.